
If You Have These Signs, You Are Having Heart Attack – Symptoms, Prevention and Medical Emergency
Overview
A heart attack occurs when the flow of blood to the heart is severely reduced or blocked. The blockage is usually due to a buildup of fat, cholesterol and other substances in the heart (coronary) arteries. The fatty, cholesterol-containing deposits are called plaques. The process of plaque buildup is called atherosclerosis.
Sometimes, a plaque can rupture and form a clot that blocks blood flow. A lack of blood flow can damage or destroy part of the heart muscle.
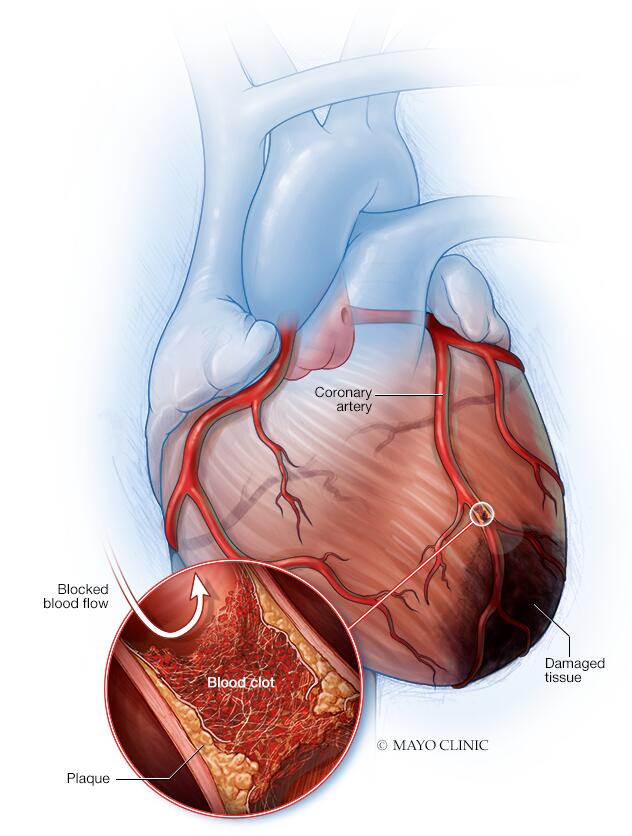
Heart attack
A heart attack occurs when an artery that sends blood and oxygen to the heart is blocked. Fatty, cholesterol-containing deposits build up over time, forming plaques in the heart’s arteries. If a plaque ruptures, a blood clot can form. The clot can block arteries, causing a heart attack. During a heart attack, a lack of blood flow causes the tissue in the heart muscle to die.
A heart attack is also called a myocardial infarction.
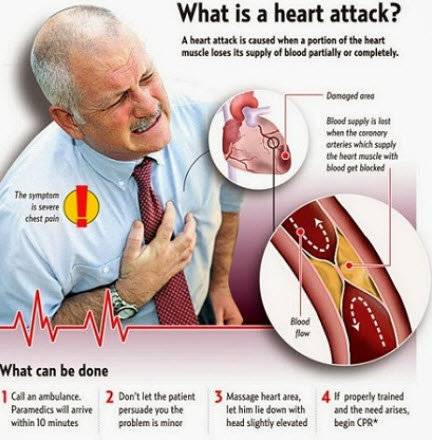
Prompt treatment is needed for a heart attack to prevent death. Call 911 or emergency medical help if you think you might be having a heart attack.
Symptoms
Symptoms of a heart attack vary. Some people have mild symptoms. Others have severe symptoms. Some people have no symptoms.
Common heart attack symptoms include:
- Chest pain that may feel like pressure, tightness, pain, squeezing or aching
- Pain or discomfort that spreads to the shoulder, arm, back, neck, jaw, teeth or sometimes the upper belly
- Cold sweat
- Fatigue
- Heartburn or indigestion
- Lightheadedness or sudden dizziness
- Nausea
- Shortness of breath
Women may have atypical symptoms such as brief or sharp pain felt in the neck, arm or back. Sometimes, the first symptom sign of a heart attack is sudden cardiac arrest.
Some heart attacks strike suddenly. But many people have warning signs and symptoms hours, days or weeks in advance. Chest pain or pressure (angina) that keeps happening and doesn’t go away with rest may be an early warning sign. Angina is caused by a temporary decrease in blood flow to the heart.

Heart attack symptoms: Know what’s a medical emergency
Whether the symptoms seem obvious or are more subtle, take them seriously and get immediate medical care.
A heart attack usually causes chest pain for more than 15 minutes. The chest pain may be mild or severe. Some people don’t have any chest pain or pressure.
Heart attack symptoms may include:
- Chest pain. It may feel like pressure, tightness, pain, squeezing or aching. The chest pain may come and go.
- Upper body pain. Pain or discomfort spreads to the shoulder, arm, back, neck, jaw, teeth or sometimes the upper belly. Some people have upper body pain with no chest discomfort.
- Shortness of breath. You may gasp for breath or try to take in deep breaths.
- Anxiety. You may feel a sense of doom or feel as if you’re having a panic attack.
- Lightheadedness or sudden dizziness. You may feel dizzy or feel like you might pass out.
- Sweating. You may suddenly break into a sweat with cold, clammy skin.
- Nausea and vomiting. You may feel sick to your stomach or throw up.
- Heartburn or indigestion. Some people who are having a heart attack may feel like they have heartburn or an upset stomach.
Older adults and people with diabetes may have no or very mild symptoms of a heart attack. Never ignore heart attack symptoms, even if they don’t seem serious.
Get help immediately
Heart attack symptoms can vary widely. For instance, you may have only mild chest discomfort while someone else has severe chest pain.
If you think that you’re having a heart attack, immediately call 911 or your local emergency number.
If you don’t have access to emergency medical services, have someone drive you to the nearest hospital. Drive yourself only if there are absolutely no other options.
Movies and TV often portray heart attacks as dramatic, chest-clutching events. But heart attacks may begin with subtle symptoms. The chest discomfort may not even be described as pain.
Many people have warning symptoms that happen hours, days or weeks in advance. For example, chest pain or pressure that keeps happening and doesn’t go away with rest may be an early warning sign of a heart attack.
When to see a doctor
Get help right away if you think you’re having a heart attack. Take these steps:
- Call for emergency medical help. If you think you’re having a heart attack, immediately call 911 or your local emergency number. If you don’t have access to emergency medical services, have someone drive you to the nearest hospital. Drive yourself only if there are no other options.
- Take nitroglycerin, if prescribed to you by a health care provider. Take it as instructed while awaiting emergency help.
- Take aspirin, if recommended. Taking aspirin during a heart attack may reduce heart damage by preventing blood clotting.
Aspirin can interact with other drugs. Don’t take an aspirin unless your care provider or emergency medical personnel say to do so. Don’t delay calling 911 to take an aspirin. Call for emergency help first.
What to do if you see someone who might be having a heart attack
If someone is unconscious and you think they’re having a heart attack, first call 911 or your local emergency number. Then check if the person is breathing and has a pulse. If the person isn’t breathing or you don’t find a pulse, only then should you begin cardiopulmonary resuscitation (CPR).

- If you’re untrained in CPR, do hands-only CPR. That means push hard and fast on the person’s chest — about 100 to 120 compressions a minute.
- If you’re trained in CPR and confident in your ability, start with 30 chest compressions before giving two rescue breaths.
Coronary artery disease causes most heart attacks. In coronary artery disease, one or more of the heart (coronary) arteries are blocked. This is usually due to cholesterol-containing deposits called plaques. Plaques can narrow the arteries, reducing blood flow to the heart.
If a plaque breaks open, it can cause a blood clot in the heart.
A heart attack may be caused by a complete or partial blockage of a heart (coronary) artery. One way to classify heart attacks is whether an electrocardiogram (ECG or EKG) shows some specific changes (ST elevation) that require emergency invasive treatment. Your health care provider may use electrocardiogram (ECG) results to describe these types of heart attacks.
- An acute complete blockage of a medium or large heart artery usually means you’ve had an ST elevation myocardial infarction (STEMI).
- A partial blockage often means you’ve had a non-ST elevation myocardial infarction (NSTEMI). However, some people with non-ST elevation myocardial infarction (NSTEMI) have a total blockage.
Not all heart attacks are caused by blocked arteries. Other causes include:
- Coronary artery spasm. This is a severe squeezing of a blood vessel that’s not blocked. The artery generally has cholesterol plaques or there is early hardening of the vessel due to smoking or other risk factors. Other names for coronary artery spasms are Prinzmetal’s angina, vasospastic angina or variant angina.
- Certain infections. COVID-19 and other viral infections may cause damage to the heart muscle.
- Spontaneous coronary artery dissection (SCAD). This life-threatening condition is caused by a tear inside a heart artery.

Risk factors
Heart attack risk factors include:
- Age. Men age 45 and older and women age 55 and older are more likely to have a heart attack than are younger men and women.
- Tobacco use. This includes smoking and long-term exposure to secondhand smoke. If you smoke, quit.
- High blood pressure. Over time, high blood pressure can damage arteries that lead to the heart. High blood pressure that occurs with other conditions, such as obesity, high cholesterol or diabetes, increases the risk even more.
- High cholesterol or triglycerides. A high level of low-density lipoprotein (LDL) cholesterol (the “bad” cholesterol) is most likely to narrow arteries. A high level of certain blood fats called triglycerides also increases heart attack risk. Your heart attack risk may drop if levels of high-density lipoprotein (HDL) cholesterol — the “good” cholesterol — are in the standard range.
- Obesity. Obesity is linked with high blood pressure, diabetes, high levels of triglycerides and bad cholesterol, and low levels of good cholesterol.
- Diabetes. Blood sugar rises when the body doesn’t make a hormone called insulin or can’t use it correctly. High blood sugar increases the risk of a heart attack.
- Metabolic syndrome. This is a combination of at least three of the following things: enlarged waist (central obesity), high blood pressure, low good cholesterol, high triglycerides and high blood sugar. Having metabolic syndrome makes you twice as likely to develop heart disease than if you don’t have it.
- Family history of heart attacks. If a brother, sister, parent or grandparent had an early heart attack (by age 55 for males and by age 65 for females), you might be at increased risk.
- Not enough exercise. A lack of physical activity (sedentary lifestyle) is linked to a higher risk of heart attacks. Regular exercise improves heart health.
- Unhealthy diet. A diet high in sugars, animal fats, processed foods, trans fats and salt increases the risk of heart attacks. Eat plenty of fruits, vegetables, fiber and healthy oils.
- Stress. Emotional stress, such as extreme anger, may increase the risk of a heart attack.
- Illegal drug use. Cocaine and amphetamines are stimulants. They can trigger a coronary artery spasm that can cause a heart attack.
- A history of preeclampsia. This condition causes high blood pressure during pregnancy. It increases the lifetime risk of heart disease.
- An autoimmune condition. Having a condition such as rheumatoid arthritis or lupus can increase the risk of a heart attack.

Complications
Heart attack complications are often due to heart muscle damage. Potential complications of a heart attack include:
- Irregular or atypical heart rhythms (arrhythmias). Heart attack damage can affect how electrical signals move through the heart, causing heartbeat changes. Some may be serious and can be deadly.
- Cardiogenic shock. This rare condition occurs when the heart is suddenly and abruptly unable to pump blood.
- Heart failure. A lot of damage to the heart muscle tissue can make the heart unable to pump blood. Heart failure can be temporary or long-lasting (chronic).
- Inflammation of the saclike tissue surrounding the heart (pericarditis). Sometimes a heart attack triggers a faulty immune system response. This condition may be called Dressler syndrome, postmyocardial infarction syndrome or postcardiac injury syndrome.
- Cardiac arrest. Without warning, the heart stops. A sudden change in the heart’s signaling causes sudden cardiac arrest. A heart attack increases the risk of this life-threatening condition. It can lead to death (sudden cardiac death) without immediate treatment.
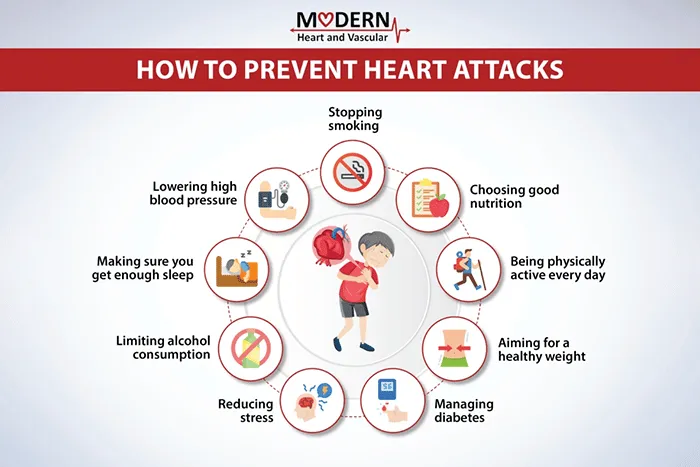
Prevention
It’s never too late to take steps to prevent a heart attack — even if you’ve already had one. Here are ways to prevent a heart attack.
- Follow a healthy lifestyle. Don’t smoke. Maintain a healthy weight with a heart-healthy diet. Get regular exercise and manage stress.
- Manage other health conditions. Certain conditions, such as high blood pressure and diabetes, can increase the risk of heart attacks. Ask your health care provider how often you need checkups.
- Take medications as directed. Your health care provider may prescribe drugs to protect and improve your heart health.
It’s also a good idea to learn CPR properly so you can help someone who’s having a heart attack. Consider taking an accredited first-aid training course, including CPR and how to use an automated external defibrillator (AED).
Can secondhand smoke increase your risk of having a heart attack?
Answer From Francisco Lopez-Jimenez, M.D.
Yes. Secondhand smoke exposure is a risk factor for having a heart attack. Secondhand smoke includes the smoke from a burning cigarette or pipe and the smoke a tobacco user breathes out.
Any amount of secondhand smoke is bad for the heart and blood vessels. Breathing secondhand smoke can cause the cells in the blood that are responsible for clotting, called platelets, to become very sticky. This makes blood more likely to clot. If a clot blocks blood flow, a heart attack or stroke can occur.
Chemicals in secondhand smoke also irritate the lining of the arteries, causing them to swell and become stiff. Such inflammation can narrow the arteries, increasing the risk of heart-related chest pain and heart attacks.
Many studies have found that heart attack rates go down in areas after smoke-free laws are passed.
To avoid secondhand smoke, try these options:
- Choose smoke-free places such as restaurants or shopping centers.
- Avoid places where people are smoking, even open spaces.
- Ask smokers in your home or whom you’re around regularly to smoke outside.
- Encourage smokers you’re often around to quit smoking.
It’s especially important to avoid secondhand smoke if you have heart disease or a history of a heart attack.
If you smoke, the best way to reduce your heart attack risk is to quit. If you need help quitting, ask your healthcare team about tips to stop smoking.


